Evelyn
February 20 6 pounds 14 ounces
A special thank you to Annica for capturing my birth photos! And for providing me with a birth timeline. Both helped me tremendously in processing through the experience and being able to recall enough to write this story.
Visit Sprout & Blossom Birth to read the story with more photographs
MONDAY, FEBRUARY 17, 2020
I had been having Braxton-Hicks contractions for months, and a couple times mid-February, I thought I might be going into labor because the contractions started to feel different — stronger, more persistent. But both times, the contractions petered out.
It wasn’t until the afternoon of Monday, February 17 — 9 days after my “guess date” — that the strong, persistent contractions stuck around. It was the real deal this time! I remembered the advice to ignore early labor until I couldn’t, so I alerted my birth team and then got busy working on a project: revamping my interior e-design website. After spending the rest of the day on that project, it didn’t seem like things were moving along too much yet, so I decided to try to get some sleep. That didn’t go as planned…back labor had set in. Back labor made it really difficult to lay down, so instead, I took shifts between eating, drinking, taking warm baths, showering, exercising on the yoga ball, walking, doing Miles Circuits, and trying to catch little naps here and there. Throughout, I implemented breathing techniques and visualized my body relaxing and opening. Loose jaw!
TUESDAY, FEBRUARY 18
Eventually, Tuesday afternoon rolled around. My contractions had intensified, and they were pretty erratic. I didn’t intend to time them, but we did here and there since they seemed so different from the patterns we’d anticipated. They’d be 8 minutes apart, then 4 minutes, then 3, then 8 again. My doula, Annica, checked in on me over the phone, and I was able to speak through most of the contractions. I decided to rely on my intuition again more than the timing of contractions. I asked my husband Matt to call Annica for me if I seemed to drift off into labor land or struggle to speak.
Walking throughout the home, this time with a hot water bottle on my belly
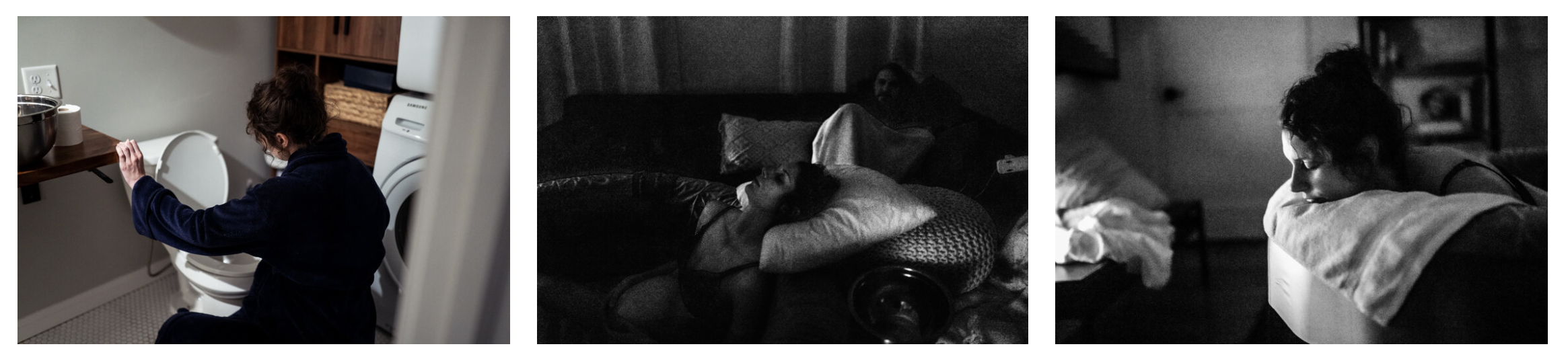
I spent most of the day pacing the house to walk through my back pain, and I rubbed my hands around my belly and breathed or vocalized through contractions. By Tuesday night, Matt sensed a shift. He asked Annica to come over, and she arrived around 11pm. My husband Matt got the birth pool ready, and I absolutely loved soaking in that between walks. I found that it was still difficult to put any pressure on my back, so I would lift myself off the ground throughout contractions in the birth pool. That was such a workout! I changed up labor positions, including laboring on the toilet, and tried to lay down again — but I popped right back up and kept walking! By midnight, I was shaky and dry heaving during contractions. I vomited. Then, my primary midwife Jen Holshoe arrived — I was so excited! Sometime after that, another midwife, Jenn DeWaard, and student midwife, Anna Stowie, arrived. It felt like things were really moving along!
WEDNESDAY, FEBRUARY 19
Tuesday became Wednesday, and I’d gone through what we thought was transition around 4am in the birth pool. My contractions had become really intense, and as predicted in our homebirth class, I had proclaimed, “I don’t know if I can keep doing this much longer!” After that, things were such a blur. I must have been deep into labor land, wading through those surges. Suddenly, everything slowed down. At first I was on cloud nine, because I thought I was experiencing what I’ve heard called “the quietude” — a period of time when the birthing person’s body takes a break before the pushing reflex kicks in. As we approached an hour of calm, my midwife Jen performed a cervical check. At 5:10am I was 8 cm dilated and baby was very low. For the next few hours, I continued to change positions, moving from laboring in the birth pool, on the toilet, on the yoga ball, in the Miles Circuit...and my contractions were pretty spaced out. I started to feel a bit concerned, because I didn’t expect labor to slow down so much for so long — especially after everything had been really intense. My midwife Jen checked my cervix again around 9am, and I was 9cm dilated — a little more on one side than the other. There were some clues that baby’s chin might not be tucked, and chin tucking/flexing is ideal for head molding and movement through the pelvis. So, we took to all the tricks to try to reposition baby!
At 11:30am, Jen helped me try to push baby past the remaining bit of cervix. We also discussed the option to rupture my membranes (AROM, artificial rupture of membranes) in hopes that this could help things progress. We tried some other positions and the Miles Circuit again, but laying down just felt so wrong and uncomfortable to me (back labor), so I didn’t get through the whole circuit. I continued to cycle through various laboring positions, and Jen checked me again around 3:00pm. Still not complete. So, we decided to give AROM a try. After the AROM, I felt a lot of pressure, but my body still wasn’t pushy, and I still wasn’t complete. I took a shower, pumped in effort to boost contractions, and got back into the birth pool.
Midwife Teresa Cramer arrived to help. We kept trying different techniques to reposition baby, including a Side Lying Release on our dining room buffet! Contractions picked up, and my spirits were lifted again, but I was growing exhausted. It was 6:00pm on Wednesday at this point, and I had been constantly moving, without sleeping, and hardly eating for about 48 hours.
By 8:00pm, the midwives could feel my baby’s head a ton! We tried to push past that remaining bit of cervix again, and when that didn’t seem to work, we decided to “push” baby back up in hopes that she would reposition with her head tucked and present ideally. That might sound intense, but I was laughing and smiling through this! My birth team was so gentle and encouraging. I stayed in “Open Knee Chest” for a while after that. About an hour later, I did a lunge-crawl from one end of the house to the other, as my birth team set pillows ahead of me along the way. I took a shower alone in the dark, and I began to cry because my body just felt so depleted. I was growing concerned, though everything was fine with baby’s heart rate. Throughout my pregnancy, I had come to believe that birth does not need to be treated as a medical event unless it becomes a medical event. I remember holding my belly in the shower, thinking, We’re stuck. This is why hospitals exist. We need to go. I had a strong feeling we should transfer to the hospital, and I started to grieve the loss of the smooth, gentle homebirth I had envisioned. I felt like I had completely exited labor land…it seemed so surreal that I had previously anticipated the shift from transition to pushing...that I had been so deep into labor land and thought that my baby’s birth was just around the corner. There I was, no longer experiencing contractions, somewhat casually packing a hospital bag.
My mom arrived to pick up our dog Islay as the rest of us prepared for the transfer.
THURSDAY, FEBRUARY 20, 2020
I transferred to the hospital just a few blocks away from our home, and my husband Matt, doula Annica, and primary midwife Jen came with me. I felt so encouraged by their presence. We arrived to our room in Labor & Delivery around 12:30am. I chose to have an epidural placed in hopes that my body could get the rest it needed. I could finally lay down comfortably. I started to feel so relaxed, and food sounded edible! Annica slipped me a granola bar, and I was so thankful to eat something.
Around 4:00am, the hospital team began to talk me through the process of Cesarean. I remember thinking, I just want my baby safe...we’re stuck...time to mentally prepare for a c-section…as, suddenly, I felt a lot of pressure. I asked them to check me again, and I was complete! The timing was wild. Over the next couple of hours, I labored in different positions on the bed. We even tried using stirrups and a squat bar — ways I truly never envisioned actively pushing my baby out. But it was working, despite her presentation. The OB came back to cheer me on as much as possible, and she even left her cell phone in the room playing bongo flava music. I remember dancing a little, in a hospital bed — so different from the quiet, private homebirth I’d anticipated! I was so thankful for the upbeat energy in the room, and it felt like just what I needed after feeling so physically depleted.
By 6:00am, my husband could see our baby’s head! By 7:00am, meconium was evident. The hospital had a shift change, and our new OB came in. Around 8:30am, I was approaching a fever, and we had the c-section talk again. The new OB told me to stop pushing, but by this point, I felt like my body couldn’t stop pushing, and I could feel that my baby was so close to being born! I requested a vacuum instead of cesarean.
They applied the vacuum to tuck baby’s chin, and in two contractions, there she was!
Our baby, Evelyn (Evie) Claire Gabriel, was born at 9:00am on Thursday, February 20, 2020. She heard her dad’s voice and spotted him out of an entire crowd. Evelyn was placed on my belly. I cried, “Oh, Evie!”, and she lifted her head and turned toward me, staring me directly in the eyes. My most favorite moment! Evie was born with very little fluid and lots of meconium, and she needed some help with suctioning and breathing. There was a NICU team on standby, and they placed Evie on CPAP. We didn’t get to have the quiet “golden hour” I’d imagined, but I felt an overwhelming sense of calm and trust that my baby was okay. I was able to hold Evie and kiss her for a little while before her dad accompanied her and the NICU team to the neonatal unit at the adjacent Children’s Hospital. I requested a placenta tour and got to see the incredible organ I grew that fostered Evelyn’s life in my womb. Then Annica showed me how to use the hospital pump, and I ordered my victory meal. I went to visit Evie in the NICU as much as I could between rest and meals in my own room. I had to be taken by wheelchair to see Evie since my body was still so physically depleted (and remained so for a couple of days). I had some concerns around being able to successfully breastfeed under those circumstances, but I advocated for nursing, asked lots of questions, and called on lactation consultants for support.
Evie’s breathing improved throughout her first day of life, and she was able to be taken off the CPAP. Evie was eager to latch, and I nursed her as often as I could. The NICU team was watching her numbers closely to determine when she was safe to be discharged. The NICU team advised formula feeding during my first stretch of nighttime sleep in the adjacent hospital, but Evie refused to take a bottle. I awoke to a phone call from the NICU, called on transport to wheel me over so Matt could keep sleeping, and eagerly rushed to Evie’s side to nurse her again. Evie’s numbers thrived when we were together and dropped when we were apart. They agreed it was best for us to stick together and determined that Evie was safe to leave the NICU. I was overjoyed! Evie was discharged from the NICU after about 24 hours, though they continued to monitor her progress from afar. We spent the afternoon together as a family of three, just soaking up the miracle of our sweet little baby. We had lots of visitors from both our homebirth team and our labor and delivery team, and we processed through the experience with every one of them. We spent our second night at the hospital together in our room, and with the support of our night nurse, we were able to get some good rest. On Saturday, February 22, we arrived home with Evie’s great-grandparents and puppy there to greet us. After Evie’s birth, I felt like superwoman! I was in absolute awe of what my body and baby were able to do throughout our days of labor!
While our birth story didn’t turn out quite how I’d envisioned, I felt incredibly empowered, and I believe that made all the difference in how I feel about the experience. And I was just so thankful that we got through everything safely, despite the rare obstacles we faced